Gwen Wagner
Post written by Gwenyth Wagner, DNP, APRN
November is National Diabetes Month.
This month, organizations across the country will band together to bring awareness about prediabetes and diabetes which affects more than 100 million U.S. Adults.
According to the Centers for Disease Control and Prevention (CDC) 30.3 million people in the United States have Diabetes, and 84.1 million people have Prediabetes.
You are at risk for developing prediabetes if you:
- Are overweight
- Are 45 years or older
- Have a parent, brother, or sister with type 2 diabetes
- Are physically active less than three times a week
- Have ever had gestational diabetes (diabetes during pregnancy) or given birth to a baby who weighed more than nine pounds
- Are African American, Hispanic/Latino American, American Indian, or Alaska Native (some Pacific Islanders and Asian Americans are also at higher risk)
The good news is that you can prevent or reverse prediabetes with lifestyle changes such as losing weight if you are overweight, eating healthier and getting regular physical activity.
If you have been diagnosed with diabetes, it is important to eat well. The first step is to make an appointment with your health care provider and discuss what changes you can make to your diet to improve your health.
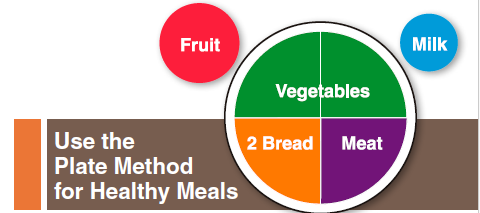
The CDC recommends that half of your nine-inch plate be filled with non-starchy vegetables like leafy greens, green beans, broccoli, cauliflower, or carrots.
One-quarter of your plate should contain lean protein such as chicken, fish or lean beef. The remaining one-quarter of your plate should contain a whole grain or starchy vegetables such as potatoes, corn, peas or winter squash. You can also eat a small amount of fresh fruit.
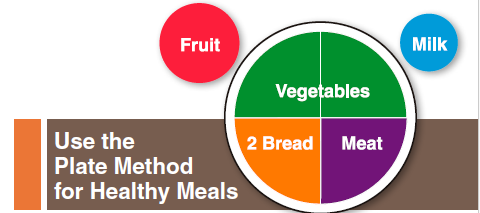
When you are grocery shopping, your cart should look like your plate. Half of your food items should be non-starchy vegetables like lettuce, asparagus, broccoli, cauliflower, cucumber, spinach, mushrooms, onions and peppers.
The rest of the cart should have lean proteins, whole grains, fruit, dairy, beans and starchy vegetables such as corn, peas, parsnips, potatoes, pumpkin, squash, zucchini and yams.
Here are a few tips to make grocery shopping easier:
- Don’t go to the store hungry.
- Make a list before you go to the store.
- Shop the perimeter of the store first. This is usually where the healthiest foods are located!
- Don’t purchase items that are not in your meal plan.
- If you have favorite foods, discuss with your dietitian, how to manage eating them occasionally.
- While at the store, don’t linger in aisles with tempting foods.
For more information and helpful tips about managing your diabetes, visit the CDC’s website at https://www.cdc.gov/diabetes/home/index.html.
To find out if you are prediabetic, take the quiz at www.preventdiabeteskc.com. This website is also a source for Diabetes Prevention Programs in the Kansas City area. Juntos provides Diabetes Prevention Classes in Spanish at HPC. Call today to find out how you can register…913-725-8676!
At HPC, we provide patient education and chronic disease management. Though dietary measures are key in prevention and can be helpful in controlling diabetes, diet changes alone are not always enough to manage this disease. Be sure to talk to your provider about what treatment is best for you. To schedule an appointment to see a provider, call 913-648-2266.
 Post written by Whitney Venegoni, APRN, FNP-C, Family Nurse Practitioner, Diabetes Clinic
Post written by Whitney Venegoni, APRN, FNP-C, Family Nurse Practitioner, Diabetes Clinic
 By:
By:  For a while we can try to forget that uncontrolled blood sugars over time will damage our eyes; block out that our provider told us we are starting to show signs of kidney damage; and pretend that the heart disease that happened to our parent (who also had diabetes) won’t happen to us!
For a while we can try to forget that uncontrolled blood sugars over time will damage our eyes; block out that our provider told us we are starting to show signs of kidney damage; and pretend that the heart disease that happened to our parent (who also had diabetes) won’t happen to us!





 As one of the leading community-based charities committed to improving the health of the greater Kansas City area, the Y wants members of our community to understand their risk for prediabetes and to take steps to avoid developing type 2 diabetes.
As one of the leading community-based charities committed to improving the health of the greater Kansas City area, the Y wants members of our community to understand their risk for prediabetes and to take steps to avoid developing type 2 diabetes.