By Maureen Caro, FNP-BC, Family Nurse Practitioner
By Maureen Caro, FNP-BC, Family Nurse Practitioner
This winter is gearing up and along with it are the cold and flu! Everyone is very concerned about COVID-19, and there is considerable overlap with symptoms from cold, flu and COVID-19. Of course, the best information comes directly from your provider! At Health Partnership Clinic, we encourage our patients to utilize the patient portal and email any questions or concerns.
A general rule of thumb for differentiating cold and flu is that you can work through a cold, but you can’t work through flu. Of course, I am not recommending anyone go to work with any kind of symptoms this year! However, people coming in pajamas and uncombed hair and falling asleep in my clinic are likely suffering from flu versus a simple cold. Flu tends to cause a fever (often high grade, over 101.3 degrees Fahrenheit), muscle aches, severe headache, fatigue. Cough, congestion, and sometimes diarrhea (more often in children) is also common. Colds tend to be more of an annoyance, a little cough, post-nasal drainage, feeling tired.
Over-the-Counter Recommendations

For over-the-counter recommendations, it depends on what symptom you are treating. For cough and nasal congestion, I prefer guaifenesin
to loosen up that drainage. The important thing is to drink a full glass of water with each dose. Guaifenesin is also called Mucinex. You can also get a product containing guaifenesin with dextromethorphan, which is abbreviated DM like Mucinex-DM, this is a cough suppressant. This can sometimes make you drowsy; I recommend it at night.
Dayquil/Nyquil are a good daytime/nighttime combination, just be sure you measure the portions! Pseudoephedrine, also called Sudafed, often abbreviated with a D at the end of the medication name, like Mucinex-D, is a good choice for nasal congestion. Sudafed can act as a mild stimulant, so it is labeled non-drowsy, but it can affect mood. I only recommend it for morning time. I also do not recommend it for anyone with hypertension or heart issues.
Sometimes people will take antihistamines to help dry up nasal drainage. Antihistamines like Benadryl (diphenhydramine, the little pink pills) are going to make you sleepy, so don’t take it and then try to work.
 As a general rule, I only like one combination product to be used at a time, like Dayquil in the morning, Nyquil in the evening, in addition to plain ibuprofen for muscle aches. It is too easy to take too much of one individual medication if you take multiple combination products. Dayquil and Nyquil both contain acetaminophen, so if you take additional acetaminophen on top of that you can damage your liver. Advil/ibuprofen is in a different drug class than Tylenol/ibuprofen, so it is fine to combine ibuprofen doses with Dayquil/Nyquil. Easiest thing to do is to ask a pharmacist when you are there at the pharmacy!
As a general rule, I only like one combination product to be used at a time, like Dayquil in the morning, Nyquil in the evening, in addition to plain ibuprofen for muscle aches. It is too easy to take too much of one individual medication if you take multiple combination products. Dayquil and Nyquil both contain acetaminophen, so if you take additional acetaminophen on top of that you can damage your liver. Advil/ibuprofen is in a different drug class than Tylenol/ibuprofen, so it is fine to combine ibuprofen doses with Dayquil/Nyquil. Easiest thing to do is to ask a pharmacist when you are there at the pharmacy!
Testing
For certainty that something is not COVID-19, the best answer is to call the clinic for a test. I have been seeing a fair amount of diarrhea/GI symptoms without a cough or nasal congestion, although cough and shortness of breath are very common. A fever over 100.4 is common, and one of the consistent symptoms I have seen is loss of smell or taste.
We have the rapid test at HPC that can be used on symptomatic patients in the first seven days of symptoms, so please call the clinic directly to see if we can schedule you for a test. Our main number is 913-648-2266. We might need to schedule you for a telemedicine visit, prior to testing, to evaluate further.
Emergency Room
 Deciding when to go to the ER, can be tricky. Any of my patients telling me they feel short of breath is always concerning. A patient that is struggling to breathe, using chest and throat muscles to breathe, or running out of air with only talking always gets me worried. A fever that cannot be controlled at home with antipyretics such as Tylenol/acetaminophen or Advil/ibuprofen, or a temperature over 103.5 degrees Fahrenheit is also a good reason to go to the ER. A child that is not drinking normally and has dry mucous membranes is also concerning, and if the parent is concerned for their child, their instincts are usually right on the nose. However, if you have a slight sore throat and/or manageable symptoms, stay home and call the clinic!
Deciding when to go to the ER, can be tricky. Any of my patients telling me they feel short of breath is always concerning. A patient that is struggling to breathe, using chest and throat muscles to breathe, or running out of air with only talking always gets me worried. A fever that cannot be controlled at home with antipyretics such as Tylenol/acetaminophen or Advil/ibuprofen, or a temperature over 103.5 degrees Fahrenheit is also a good reason to go to the ER. A child that is not drinking normally and has dry mucous membranes is also concerning, and if the parent is concerned for their child, their instincts are usually right on the nose. However, if you have a slight sore throat and/or manageable symptoms, stay home and call the clinic!
References:
https://www.cdc.gov/flu/symptoms/coldflu.htm


 By:
By:  Stay home if you are sick.
Stay home if you are sick. By
By  Depending on the age of your child, write down or have them write down everything they have to do to get ready for school. Be very detailed. Have them practice doing these things and time them to make it a game.
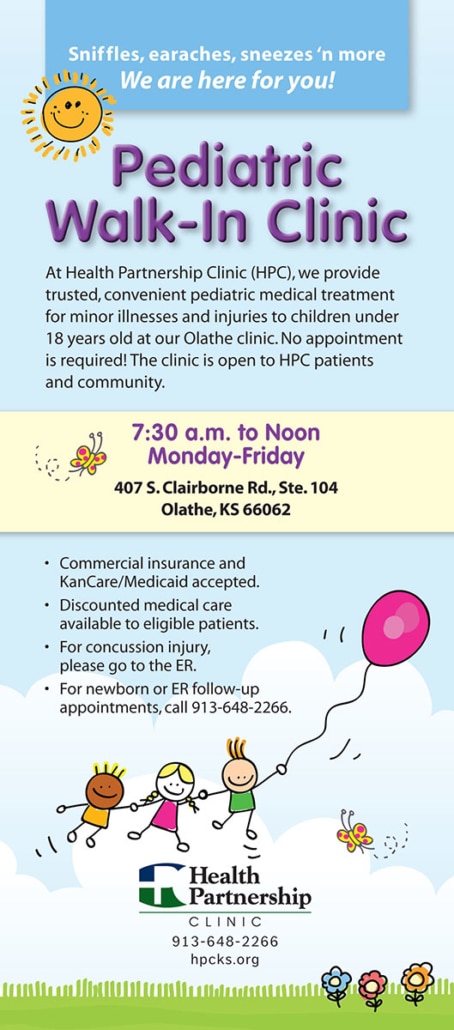
Depending on the age of your child, write down or have them write down everything they have to do to get ready for school. Be very detailed. Have them practice doing these things and time them to make it a game. Health Partnership Clinic offers back-to-school and sports physicals at all our clinic sites, including Olathe, Shawnee Mission, Paola and Ottawa. At the Olathe site, we offer a Walk-In Pediatric Clinic, Monday-Friday from 7:30 a.m. to Noon.
Health Partnership Clinic offers back-to-school and sports physicals at all our clinic sites, including Olathe, Shawnee Mission, Paola and Ottawa. At the Olathe site, we offer a Walk-In Pediatric Clinic, Monday-Friday from 7:30 a.m. to Noon. Most importantly, wash your hands on a regular basis (before eating, after eating, after using the restroom, etc.) and sneeze in your arms not in your hands.
Most importantly, wash your hands on a regular basis (before eating, after eating, after using the restroom, etc.) and sneeze in your arms not in your hands. We are participating in the Federal program to distribute COVID-19 Home Testing Kits. You can pick up kits at our clinic locations by asking the front desk. Limit two per household member.
We are participating in the Federal program to distribute COVID-19 Home Testing Kits. You can pick up kits at our clinic locations by asking the front desk. Limit two per household member. By
By  A: I believe in each of the COVID vaccines. Many of the vaccine manufacturers have been studying their effects in children and young adults for several months prior to their recent approval. I agree with the Centers for Disease Control and Prevention’s (CDC) recent approval of vaccinating individuals 12 and over. I believe the regulators have done a nice job of balancing the benefits of vaccination with a measure of deliberateness needed to make sure each vaccine is safe in younger age groups. Bottom line: I would not hesitate to give my own child a vaccine approved for use by the CDC.
A: I believe in each of the COVID vaccines. Many of the vaccine manufacturers have been studying their effects in children and young adults for several months prior to their recent approval. I agree with the Centers for Disease Control and Prevention’s (CDC) recent approval of vaccinating individuals 12 and over. I believe the regulators have done a nice job of balancing the benefits of vaccination with a measure of deliberateness needed to make sure each vaccine is safe in younger age groups. Bottom line: I would not hesitate to give my own child a vaccine approved for use by the CDC. By
By 
 As a general rule, I only like one combination product to be used at a time, like Dayquil in the morning, Nyquil in the evening, in addition to plain ibuprofen for muscle aches. It is too easy to take too much of one individual medication if you take multiple combination products. Dayquil and Nyquil both contain acetaminophen, so if you take additional acetaminophen on top of that you can damage your liver. Advil/ibuprofen is in a different drug class than Tylenol/ibuprofen, so it is fine to combine ibuprofen doses with Dayquil/Nyquil. Easiest thing to do is to ask a pharmacist when you are there at the pharmacy!
As a general rule, I only like one combination product to be used at a time, like Dayquil in the morning, Nyquil in the evening, in addition to plain ibuprofen for muscle aches. It is too easy to take too much of one individual medication if you take multiple combination products. Dayquil and Nyquil both contain acetaminophen, so if you take additional acetaminophen on top of that you can damage your liver. Advil/ibuprofen is in a different drug class than Tylenol/ibuprofen, so it is fine to combine ibuprofen doses with Dayquil/Nyquil. Easiest thing to do is to ask a pharmacist when you are there at the pharmacy! Deciding when to go to the ER, can be tricky. Any of my patients telling me they feel short of breath is always concerning. A patient that is struggling to breathe, using chest and throat muscles to breathe, or running out of air with only talking always gets me worried. A fever that cannot be controlled at home with antipyretics such as Tylenol/acetaminophen or Advil/ibuprofen, or a temperature over 103.5 degrees Fahrenheit is also a good reason to go to the ER. A child that is not drinking normally and has dry mucous membranes is also concerning, and if the parent is concerned for their child, their instincts are usually right on the nose. However, if you have a slight sore throat and/or manageable symptoms, stay home and call the clinic!
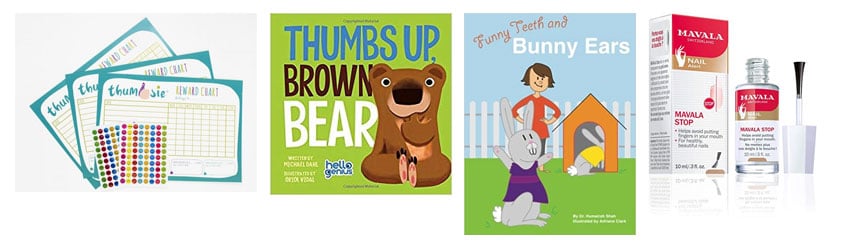
Deciding when to go to the ER, can be tricky. Any of my patients telling me they feel short of breath is always concerning. A patient that is struggling to breathe, using chest and throat muscles to breathe, or running out of air with only talking always gets me worried. A fever that cannot be controlled at home with antipyretics such as Tylenol/acetaminophen or Advil/ibuprofen, or a temperature over 103.5 degrees Fahrenheit is also a good reason to go to the ER. A child that is not drinking normally and has dry mucous membranes is also concerning, and if the parent is concerned for their child, their instincts are usually right on the nose. However, if you have a slight sore throat and/or manageable symptoms, stay home and call the clinic! While thumb sucking is undeniably adorable the first couple of years, as kindergarten approaches and those front teeth start bucking out, parents can easily start to panic!
While thumb sucking is undeniably adorable the first couple of years, as kindergarten approaches and those front teeth start bucking out, parents can easily start to panic!





 Some common causes of allergic asthma are allergens small enough to be breathed into the lungs such as:
Some common causes of allergic asthma are allergens small enough to be breathed into the lungs such as: