Post by Sierra Miller, Kansas City University of Medical Biosciences, DO/MA candidate 2021
Post by Sierra Miller, Kansas City University of Medical Biosciences, DO/MA candidate 2021
Changing the Narrative
Healthcare is one of the most divisive and partisan topics in the current political climate. Most people can tell you a horror story of a long ER wait, an enormous medical bill, or some other way the healthcare system has failed them. But what you don’t commonly hear about are the amazing ways that healthcare can improve the life of a person, family or community.
Collectively we have a tendency to ignore things when they are going as we expect them to and focus on the negative or bothersome things that are interrupting our plans. We don’t usually think about the shoes on our feet, until they are causing a blister. Similarly, we are quick to double down on our own opinions when someone expresses an idea that seems different from our own. These reactions have brought us to a point where nearly everyone is dissatisfied with the current system in place, but we seem unable to have a productive conversation about approaches to improve the healthcare system.
Where We Agree
Today, I want to change that narrative and instead of focusing on where we differ in our approach to healthcare policy, I want to talk about where we are more likely to agree.
- One thing we are all likely to agree on is that we don’t want to wait for seven hours in the waiting room of the local ER and then receive a bill for $2,500.
- We don’t want to have to pay more than a $1,000 a month for prescription medications that are required to keep us alive.
- We want to know that when we need healthcare we have quick and affordable access to it, and we want to know that the care we seek will be safe and effective.
- And we also want to know that if we make any changes to the current system that we will benefit from those changes.
If you are shaking you head in agreement with me so far, don’t lose faith when you read the next sentence, hear me out. I believe that the first step toward improving all of these things is through supporting community health programs.
Community Health
When I use the term “community health” I intend to describe the intersection where both the medical and social needs of a group of people within a specific geographic area are met. The health of a community affects everyone who lives or works within it, including you. The community you live in affects your everyday life in more ways than you may realize.
You may not be the person who participates in the annual neighborhood garage sale or volunteers with the PTA, but chances are you do drive on the roads and go to the local grocery store. The health of your community impacts the safety of the roads you drive on, crime rates, educational opportunities, neighborhood green spaces, transportation options, what businesses are willing to operate in your neighborhood and therefore what resources you have access to.
Most of us can identify a few things in our own neighborhoods that we would wish to improve. My ask today, is that when considering how to improve the community you live in, you consider the importance of the health of the members within your community.
Improving the Team
 Analogous to a sports team, a community is only as strong as the weakest players. If we want to improve the team, we can see the biggest gains by investing in the players who have the most room for improvement. Community Health Centers (CHC) like Health Partnership Clinic are designed to improve the health of the communities they serve. They function by partnering community resources and federal funding to make healthcare more accessible and affordable for the medically underinsured population.
Analogous to a sports team, a community is only as strong as the weakest players. If we want to improve the team, we can see the biggest gains by investing in the players who have the most room for improvement. Community Health Centers (CHC) like Health Partnership Clinic are designed to improve the health of the communities they serve. They function by partnering community resources and federal funding to make healthcare more accessible and affordable for the medically underinsured population.
They provide more than just access to a primary care physician, they also bring improved access to dental care, behavioral healthcare and many other social health services.
Right now, you might be thinking I have insurance, I can pay my bills, or I don’t need this in my neighborhood. I assure you that improving the access for those who might be one paycheck or medical bill away from not being able to pay their rent will have trickle down effects to services you do use.
The Community Health Center Model
The Community Health Center (CHC) model was brought to the United States in the 1950s by Dr. Geiger. From its inception, the CHC model has proven to have compounding health effects throughout all areas of the communities that they serve. They allow patients continuity of care and improved management of chronic diseases such as diabetes and heart disease.
According to The Centers for Disease Control and Prevention (CDC), 90 percent of the $3.3 trillion spent on annual healthcare expenses goes toward managing chronic and mental health conditions.
Helping patients manage these diseases in a primary care setting reduces disease progression and complications rates. Appropriate management of these conditions in an outpatient setting also helps to relieve hospitals from having to function as a primary care physicians office and reduces some of the dramatic economic burden associated with managing chronic diseases in an acute setting. This means reduced costs, reduced waiting time, reduced physician burnout, reduced morbidity and mortality.
This also means that when you have healthy members in your community, you have more people who can contribute to the economy. You see healthier children who are more prepared for their education and to become future contributing members of society. When there is stronger economic strength you also see lower crime rates, more development and improved quality of life.
Solutions to our Biggest Problems
I truly believe that improving community health is vital to changing the narrative we are hearing and experiencing in today’s healthcare system. That is why as a third-year medical student I have chosen to work in community health centers and plan to become a primary care physician. I want to be able to serve my community and be part of the solution. I believe that focusing on our shared interests is the only way forward if we want to change the current healthcare climate and improve the communities that we live in.
When we do this, I believe the solutions to many of our biggest problems will also start to fall into place.
Sierra Miller is a third-year Osteopathic Medical Student at Kansas City University of Medicine and Biosciences in the Community Health Center Track and is a dual degree student completing her Masters in Bioethics. Sierra has completed two months of rotations as a student in the areas of Family Medicine and Community Health Center Administration at Health Partnership Clinic in Olathe.
 By Pauline Shaver, MSW Practicum Student, University of Kansas
By Pauline Shaver, MSW Practicum Student, University of Kansas As well as recognizing the diverse experiences within ASD community, acknowledgement of common barriers those diagnosed may face within neurotypical environments is essential. Within service provision and educational settings, research indicates a consistent presence of “misconceptions and inadequate knowledge about autism.” In addition to factual fallacies about the diagnosis, a pervasive lack of understanding about supportive practices creates environments which are unresponsive to the unique needs of those with ASD. This serves to further stigmatize autism spectrum disorder, as individuals with ASD are often perceived negatively in unsupportive and uninformed spaces.
As well as recognizing the diverse experiences within ASD community, acknowledgement of common barriers those diagnosed may face within neurotypical environments is essential. Within service provision and educational settings, research indicates a consistent presence of “misconceptions and inadequate knowledge about autism.” In addition to factual fallacies about the diagnosis, a pervasive lack of understanding about supportive practices creates environments which are unresponsive to the unique needs of those with ASD. This serves to further stigmatize autism spectrum disorder, as individuals with ASD are often perceived negatively in unsupportive and uninformed spaces.





 By Marissa Alcantar, Storybank and Policy Specialist with Alliance for a Healthy Kansas
By Marissa Alcantar, Storybank and Policy Specialist with Alliance for a Healthy Kansas The HHA Program is a four-month program to encourage self-monitoring and recording of blood pressure, as well as a heart-healthy diet.
The HHA Program is a four-month program to encourage self-monitoring and recording of blood pressure, as well as a heart-healthy diet.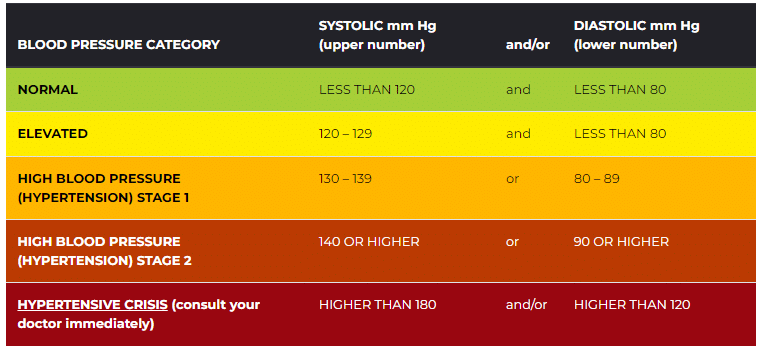







 Post written by
Post written by 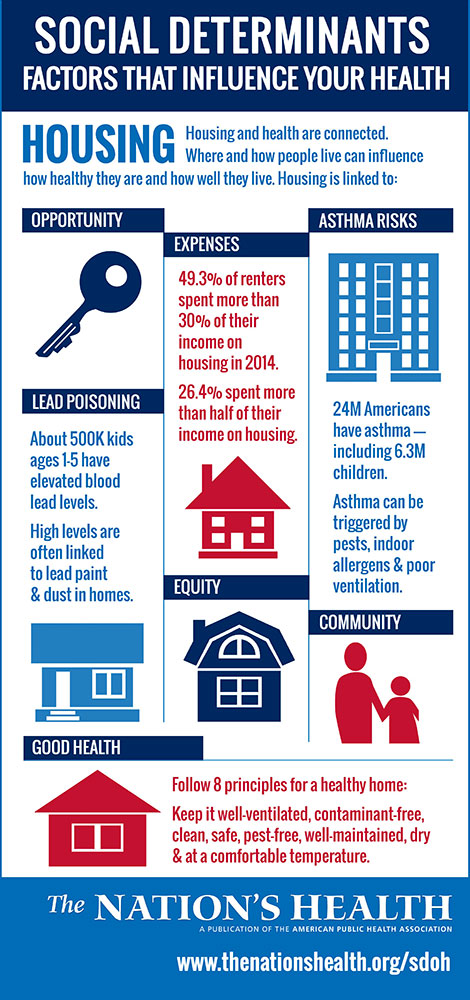 How does stress impact our health and overall well-being? Approximately one in five community members reported experiencing physical symptoms (upset stomach, headache, etc.) due to their finances sometimes, usually or always in the past 12 months.
How does stress impact our health and overall well-being? Approximately one in five community members reported experiencing physical symptoms (upset stomach, headache, etc.) due to their finances sometimes, usually or always in the past 12 months.