National Patient Safety Awareness Week – Safe Care Key at Health Partnership Clinic
 By Mindy Beckwith, MSN, RN, Clinic Director/Risk Manager at Health Partnership Clinic
By Mindy Beckwith, MSN, RN, Clinic Director/Risk Manager at Health Partnership Clinic
At Health Partnership Clinic (HPC) we are committed to providing safe, value-based care to all. During National Patient Safety Awareness Week, March 10-16, we want to take the opportunity to share a couple of ways we are keeping our patients safe.
We strive to improve the health of our patients and the community we serve.
A big component of providing safe care is understanding the importance of reporting near misses and events that occur outside of normal expectations, also known as an occurrence. Learning from occurrences and not assigning blame is paramount in finding the root cause of why these events happened.
Making mistakes is part of being human. Most people have never gone through a day without making some mistakes. Most mistakes generally occur with no harm, however, mistakes in health care are not always that way. When making a mistake or recognizing an event could potentially lead to harm, reporting quickly is imperative. At HPC we use collected data to help our organization make informed decisions about process improvements, training needs, resource allocation, and risk management.
Electronic Reporting System
 Recently we adopted and implemented an electronic reporting system, which includes an easy way to report occurrences that are outside of the normal, expected operations of the day. This system provides an easy, efficient way to report occurrences and provides data that leads to both enhanced patient safety and better patient outcomes.
Recently we adopted and implemented an electronic reporting system, which includes an easy way to report occurrences that are outside of the normal, expected operations of the day. This system provides an easy, efficient way to report occurrences and provides data that leads to both enhanced patient safety and better patient outcomes.
Here at HPC, we are constantly looking for new and improved ways to provide safe care to patients and their families. With the implementation of better reporting systems and comprehensive reviews of opportunities for improvement, we can realize a better understanding of keeping patients and our community safe.
The clinic welcomes new patients. To schedule an appointment, call 913-648-2266 today! To learn more about our services, visit us at hpcks.org.


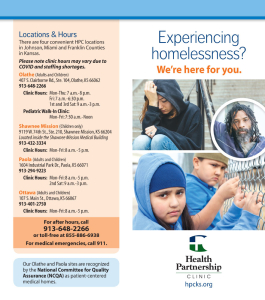
 The Mobile Integrated Health (MIH) Team, a partnership between the clinic, Olathe Fire Department and Olathe Health, brings care to Olathe patients in their homes and out in the community to break down barriers to care. This service is available only to Olathe residents. To access non-emergency care, call MIH at 913-334-8228.
The Mobile Integrated Health (MIH) Team, a partnership between the clinic, Olathe Fire Department and Olathe Health, brings care to Olathe patients in their homes and out in the community to break down barriers to care. This service is available only to Olathe residents. To access non-emergency care, call MIH at 913-334-8228. By
By  Respiratory Syncytial Virus (RSV)
Respiratory Syncytial Virus (RSV) Updated COVID-19 vaccines were approved on September 11, 2023. The new vaccine was authorized for six months and older, and everyone ages six months and older is recommended to receive at least one dose this year (if it has been at least two months since your last COVID vaccine). Vaccines will soon be available at HPC for all our patients and staff regardless of insurance status. Remember the best way to avoid severe COVID-19 infection is to stay up to date with vaccines.
Updated COVID-19 vaccines were approved on September 11, 2023. The new vaccine was authorized for six months and older, and everyone ages six months and older is recommended to receive at least one dose this year (if it has been at least two months since your last COVID vaccine). Vaccines will soon be available at HPC for all our patients and staff regardless of insurance status. Remember the best way to avoid severe COVID-19 infection is to stay up to date with vaccines. By
By  If you find yourself stuck asking the “why” questions, that is a great reminder and opportunity to pause, observe, and engage in the following:
If you find yourself stuck asking the “why” questions, that is a great reminder and opportunity to pause, observe, and engage in the following:

















 By
By