By Amy Gray, LSCSW, Behavioral Health Clinician
By Amy Gray, LSCSW, Behavioral Health Clinician
Self-Care
Self-care almost always evokes an image for people, whether it be a hot bath, a vacation, or pampering in some way. Self-care is not one-size-fits-all and can come in all shapes and sizes. Some people are filled up by meditation or yoga, others prefer walking in the woods or journaling. Self-care requires time and attention and focus, is developed over time, and should be a part of our regular routine to keep ourselves healthy and mentally strong. Self-care is an act, a habit, or a practice.
There are several types or categories of self-care, including: Emotional, Mental, Physical, Pleasure, Sensory, Social, and Spiritual.
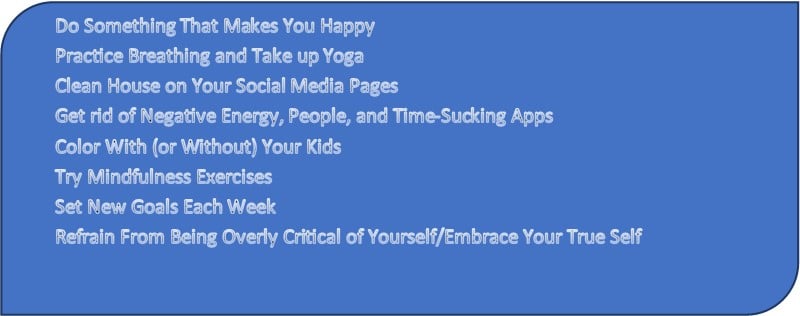
Emotional Self-Care Ideas
The website www.developgoodhabits.com identifies the following Emotional Self-Care Ideas:
Emotional Wellness
 Emotional wellness is difficult in our world in a regular year, yet during a pandemic year, the obstacles can seem monumental. Break things down into doable steps. Ask for help when needed. Cry if you need to, and use grounding to keep focused. There is no precedence for how you should respond in times like this, it is a pandemic and nothing about that is natural.
Emotional wellness is difficult in our world in a regular year, yet during a pandemic year, the obstacles can seem monumental. Break things down into doable steps. Ask for help when needed. Cry if you need to, and use grounding to keep focused. There is no precedence for how you should respond in times like this, it is a pandemic and nothing about that is natural.
Physical self-care is important for mental and emotional health and aids in sleep and eating habits. Motivation might be hard to come by, start small and get moving. Social self-care allows us to connect with others. Finding ways to spend time with people (via social media apps, social distancing, etc.) is important. Spending time in prayer or at online church services can mitigate the loss of church family, church events and spiritual practices. In all areas important to you, try to make new traditions that feed your needs and raise your spirits.
…In A Pandemic!!
 In the past year, many people have struggled due to the changes COVID19 has made to our daily lives. Our safety and security has been threatened by a very real virus, and mental health effects have been significant. An increase in anxiety, depression, alcohol and drug use, and relationship issues have been evident in the patients seen at Health Partnership. Patients who have never experienced anxiety and depression are reporting problems for the first time, and many patients with a history are reporting a significant increase in symptoms.
In the past year, many people have struggled due to the changes COVID19 has made to our daily lives. Our safety and security has been threatened by a very real virus, and mental health effects have been significant. An increase in anxiety, depression, alcohol and drug use, and relationship issues have been evident in the patients seen at Health Partnership. Patients who have never experienced anxiety and depression are reporting problems for the first time, and many patients with a history are reporting a significant increase in symptoms.
More than one-third of Americans have displayed clinical signs of anxiety, depression, or both since the coronavirus pandemic began.
The American Psychological Association (which typically issues an annual mental health survey) has been releasing a monthly report, Stress in America 2020: Stress in the Time of COVID-19.
 According to PEW Research, one-third of Americans (33 percent) have experienced high levels of psychological distress at some point during the extended period of social distancing undertaken to slow the spread of COVID-19, the disease caused by the novel coronavirus. More than half (55 percent) of adults who describe their financial situation as poor have experienced high levels of distress, as have half of those who report having a disability or handicap that keeps them from fully participating in work, school or other activities.
According to PEW Research, one-third of Americans (33 percent) have experienced high levels of psychological distress at some point during the extended period of social distancing undertaken to slow the spread of COVID-19, the disease caused by the novel coronavirus. More than half (55 percent) of adults who describe their financial situation as poor have experienced high levels of distress, as have half of those who report having a disability or handicap that keeps them from fully participating in work, school or other activities.
It is important to normalize the effects a global pandemic, including widespread shutdowns and stay-at-home orders, remote-only school attendance and the loss of connection that people are experiencing. Weddings have been canceled or rescheduled. Funerals have been delayed or family members have been unable to travel to say goodbye. Baby showers and birthday parties and bar mitsvahs and graduations and anniversaries and holidays…the list goes on and on. In a global pandemic, the rules change, and “normal” is simplified and redefined. In a pandemic, the main goal is survival.
Dr. Joy Osofsky in Psychology Today writes: “Self-care is crucial to support health and mental health, which starts with establishing regular routines for this “new normal” environment that include getting enough sleep, eating regular meals, exercise and making connections virtually with family and friends.”
Helpful Hints for Surviving, or Even Thriving, in a Pandemic
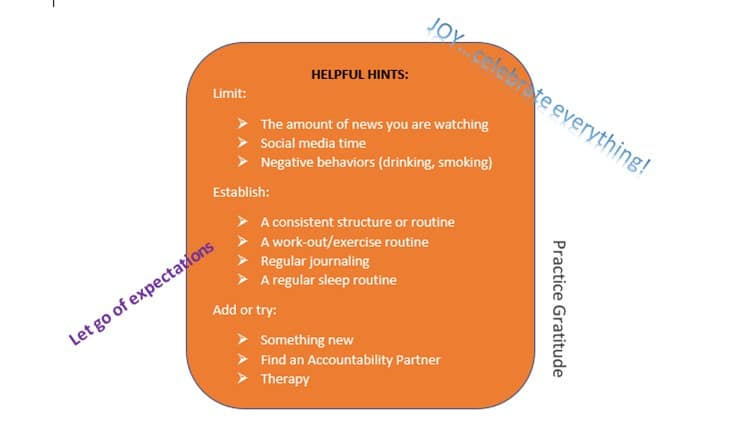
ADAPT: Individual self-care in a pandemic needs to adapt to the current circumstances. Work on making small changes, don’t try to change everything all at once. Set a daily or weekly goal and find JOY in celebrating the small wins and good efforts you make.
GRATITUDE: Practice gratitude by journaling 5 good things that have happened, and/or make sticky notes and place them on your bathroom mirror as a reminder of positive things happening.
PROPS: A bright light or light box are used for Seasonal Affective Disorder (SAD) and mimic daylight, which can be very helpful for people who get down during the dark winter months. As little as 10 minutes a day can help lift your mood. Finding light, in a light box, a conversation, or at the end of this very long pandemic tunnel, is critical.
JOY: Find some JOY….and celebrate everything!!! Celebrate getting the laundry done, getting out of bed, feeding yourself healthy food, and making time for self-care activities. Celebrating helps focus on success and progress. Practice gratitude and celebrate surviving the year 2020.
PRACTICE…PRACTICE…PRACTICE
 The New Year can be a challenging time as well as a time for hope. Often, the New Year is associated with celebrations, resolutions, and higher expectations for ourselves, and life in general. This can be energizing, or it may feel overwhelming, especially for those of us whose spirits are weary from the pressures of the past year. For this reason, it is important to consider how we can recharge our spirts and nurture our well-being while looking for ways to grow in the coming year.
The New Year can be a challenging time as well as a time for hope. Often, the New Year is associated with celebrations, resolutions, and higher expectations for ourselves, and life in general. This can be energizing, or it may feel overwhelming, especially for those of us whose spirits are weary from the pressures of the past year. For this reason, it is important to consider how we can recharge our spirts and nurture our well-being while looking for ways to grow in the coming year.
 Behind the statistics there are countless stories of those impacted by serious mental illness. Limited resources for responding to mental health crises can have tragic results. In many cases ineffective crisis response results in traumatization of the person suffering from a mental health crisis, as well as traumatic impacts on loved ones, friends and crisis responders. In some cases, the crisis may lead to serious injury or death of the person experiencing the mental health crisis, and risk of injury or death of crisis responders. Communities, including many in the Kansas City region, are seeking to improve their responses to mental health needs through use of law-enforcement Crisis Intervention Teams (CIT), mental health co-responders to assist police and the addition of social service workers to police departments.
Behind the statistics there are countless stories of those impacted by serious mental illness. Limited resources for responding to mental health crises can have tragic results. In many cases ineffective crisis response results in traumatization of the person suffering from a mental health crisis, as well as traumatic impacts on loved ones, friends and crisis responders. In some cases, the crisis may lead to serious injury or death of the person experiencing the mental health crisis, and risk of injury or death of crisis responders. Communities, including many in the Kansas City region, are seeking to improve their responses to mental health needs through use of law-enforcement Crisis Intervention Teams (CIT), mental health co-responders to assist police and the addition of social service workers to police departments.


 By
By 
 It’s perfectly natural to feel anxious, stressed or frustrated when there is uncertainty in your life. For some people, that mental toll may lead to pervasive anxiety or even depression. It’s been a stressful year for some, and it’s important to know, you are not struggling alone.
It’s perfectly natural to feel anxious, stressed or frustrated when there is uncertainty in your life. For some people, that mental toll may lead to pervasive anxiety or even depression. It’s been a stressful year for some, and it’s important to know, you are not struggling alone. Find hobbies or activities that also can help you relax. Try deep breathing, stretching or meditation. Reading books, drawing or doing puzzles can also be calming.
Find hobbies or activities that also can help you relax. Try deep breathing, stretching or meditation. Reading books, drawing or doing puzzles can also be calming. Take Care. Find articles, self-care tools, caring providers, and more mental health and substance use resources at
Take Care. Find articles, self-care tools, caring providers, and more mental health and substance use resources at  By Amy Gray, LSCSW, Behavioral Health Clinician
By Amy Gray, LSCSW, Behavioral Health Clinician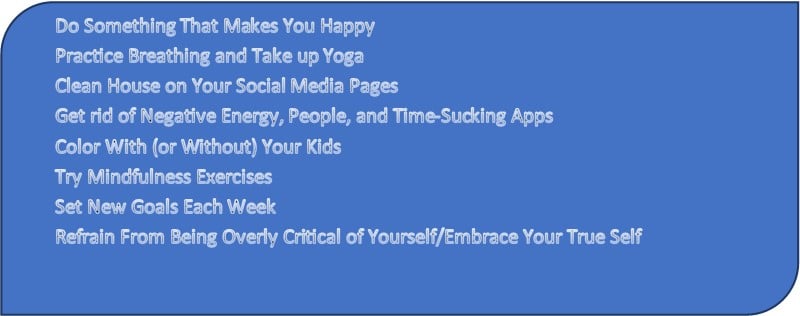
 Emotional wellness is difficult in our world in a regular year, yet during a pandemic year, the obstacles can seem monumental. Break things down into doable steps. Ask for help when needed. Cry if you need to, and use grounding to keep focused. There is no precedence for how you should respond in times like this, it is a pandemic and nothing about that is natural.
Emotional wellness is difficult in our world in a regular year, yet during a pandemic year, the obstacles can seem monumental. Break things down into doable steps. Ask for help when needed. Cry if you need to, and use grounding to keep focused. There is no precedence for how you should respond in times like this, it is a pandemic and nothing about that is natural. In the past year, many people have struggled due to the changes COVID19 has made to our daily lives. Our safety and security has been threatened by a very real virus, and mental health effects have been significant. An increase in anxiety, depression, alcohol and drug use, and relationship issues have been evident in the patients seen at Health Partnership. Patients who have never experienced anxiety and depression are reporting problems for the first time, and many patients with a history are reporting a significant increase in symptoms.
In the past year, many people have struggled due to the changes COVID19 has made to our daily lives. Our safety and security has been threatened by a very real virus, and mental health effects have been significant. An increase in anxiety, depression, alcohol and drug use, and relationship issues have been evident in the patients seen at Health Partnership. Patients who have never experienced anxiety and depression are reporting problems for the first time, and many patients with a history are reporting a significant increase in symptoms.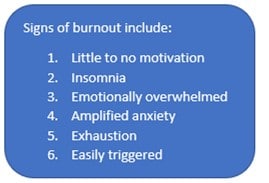 According to PEW Research, one-third of Americans (33 percent) have experienced high levels of psychological distress at some point during the extended period of social distancing undertaken to slow the
According to PEW Research, one-third of Americans (33 percent) have experienced high levels of psychological distress at some point during the extended period of social distancing undertaken to slow the 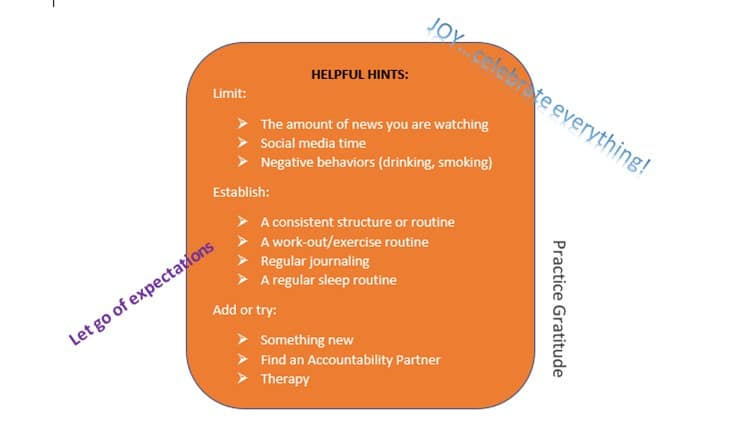
 By Tristen Winston, MA, PsyD, LP, LCAC, Licensed psychologist and Behavioral Health Director, Health Partnership Clinic
By Tristen Winston, MA, PsyD, LP, LCAC, Licensed psychologist and Behavioral Health Director, Health Partnership Clinic
 Stay connected to family and friends virtually
Stay connected to family and friends virtually
 Post written by Delanie Barnard, MA, Kansas City University, Doctoral Candidate
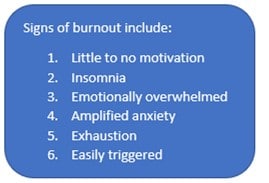
Post written by Delanie Barnard, MA, Kansas City University, Doctoral Candidate What can you do if someone you know is showing these warning signs?
What can you do if someone you know is showing these warning signs?