It’s National Domestic Violence Awareness Month! Don’t stay silent. Educate yourself and speak up.
By Catherine Rice, Vice President of Marketing/Outreach
October is National Domestic Violence Awareness Month, which first began in 1981 by the National Coalition Against Domestic Violence as a Day of Unity to connect battered women’s advocates across the country. Domestic violence affects millions, both women and men, of every race, religion, culture and status. It’s not just punches and black eyes — it’s yelling, humiliation, stalking, manipulation, coercion, threats and isolation. It’s stealing a paycheck, keeping tabs online, non-stop texting, the constant use of silent treatment, or calling someone stupid so often they believe it.
Since the Violence Against Women Act passed in 1994, we’ve come a long way.
This landmark legislation, led by then Senator Joe Biden, combined new provisions that hold offenders accountable and provide programs and services for victims. Between 1993 and 2010, the overall rate of domestic violence dropped nearly two-thirds and state laws have reformed to address issues such as dating abuse in the workplace, stalking, employment discrimination and more.
Nearly three out of four Americans personally know someone who is or has been a victim of domestic violence. And unfortunately, no one knows better of the traumatic impact than our very own Kallie Weas, MA.
Kallie’s Story
 Kallie’s 23-year-old sister, Katie, and six-month-old niece were killed on Oct. 23, 2013 by Katie’s abuser-boyfriend. Last week, staff wore purple in support of Domestic Violence Month and Kallie and her family. Kallie’s family is celebrating their seventh-year anniversary. Purple ribbons were distributed to patients and staff.
Kallie’s 23-year-old sister, Katie, and six-month-old niece were killed on Oct. 23, 2013 by Katie’s abuser-boyfriend. Last week, staff wore purple in support of Domestic Violence Month and Kallie and her family. Kallie’s family is celebrating their seventh-year anniversary. Purple ribbons were distributed to patients and staff.
“My sister and her baby daughter were killed by her abuser via a head on collusion,” Kallie reflects. “This was so devastating for all of us, including the innocent man driving the other car, who survived. To heal and remember Katie and her daughter, we launch a balloon for each year she and her daughter are no longer with us. In addition, my sister and I focus on educating people about domestic abuse.”
Kallie approached her supervisor, Lee Champion, RN, Clinic Director/Risk and Compliance Officer, and CEO Amy Falk, about bringing more awareness about domestic abuse to HPC.
“We often only associate October with “pink” and Breast Cancer Awareness Month,” Amy adds. “But for those impacted by domestic violence, including family members of the abused, National Domestic Violence Awareness Month is an opportunity to educate and bring awareness of this important public health priority. We applaud Kallie’s efforts to encourage conversation about this issue.”
Kallie can’t agree more. “I felt the best way to honor my sister is to make sure my colleagues, friends, patients and community better understand the signs of domestic abuse and what to do if a person is being abused. My older sister posts daily stats and information about domestic violence on social media. We each do something in our own way. I just want our staff and patients to know the signs and think about this issue—and not have to live through our nightmare.”
Kallie urges everyone to become informed, know the signs and take a stand. Please support survivors (and their families like Kallie’s) and speak out against domestic violence – not just in October but year-round.
Did you know?
- The U.S. Department of Justice estimates that 1.3 million women and 835,000 men are victims of physical violence by a partner every year.
- Every nine seconds, a woman in the U.S. is beaten or assaulted by a current or ex-significant other.
- One in four men are victims of some form of physical violence by an intimate partner.
Why do people in an abusive relationship stay with their partners?
There are a few reasons:
- Their self-esteem is destroyed, and they are made to feel they will never be able to find another person to be with.
- The cycle of abuse, meaning the ‘honeymoon phase’ that follows physical and mental abuse, makes them believe their partner really is sorry and does love them.
- It’s dangerous to leave. Women are 70 times more likely to be killed in the weeks after leaving their abusive partner than at any other time in the relationship, according to the Domestic Violence Intervention program.
- Statistics suggest that almost five percent of male homicide victims each year are killed by an intimate partner.
- They feel personally responsible for their partner, or their own behavior. They are made to feel like everything that goes wrong is their fault.
- They share a life. Marriages, children, homes, pets and finances are reasons victims of abuse feel they can’t leave.
Are you in an abusive relationship?
Sometimes, people don’t know if they are really in an abusive relationship because they’re used to their partner calling them crazy or making them feel like all the problems are their own fault.
Here are a few ways to know if you’re in an abusive relationship that you need to get out of.
- Your partner has hit you, beat you, or strangled you in the past.
- Your partner is possessive. They check up on you constantly wondering where you are; they get mad at you for hanging out with certain people if you don’t do what they say.
- Your partner is jealous. (A small amount of jealousy is normal and healthy) however, if they accuse you of being unfaithful or isolate you from family or friends, that means the jealousy has gone too far.
- Your partner puts you down. They attack your intelligence, looks, mental health, or capabilities. They blame you for all their violent outbursts and tell you nobody else will want you if you leave.
- Your partner threatens you or your family.
- Your partner physically and sexually abuses you. If they EVER push, shove, or hit you, or make you have sex with them when you don’t want to, they are abusing you (even if it doesn’t happen all the time.)
Signs Someone You Know Is Being Abused
Keep an eye out for things like:
- Excuses for injuries
- Personality changes, like low self-esteem in someone who was always confident
- Constantly checking in with their partner
- Never having money on hand
- Overly worried about pleasing their partner
- Skipping out on work, school, or social outings for no clear reason
- Wearing clothes that don’t fit the season, like long sleeves in summer to cover bruises
Are the Signs Different for Men?
They’re often the same. And that’s true whether the abusive partner is a woman or another man. It may be emotional or verbal, like taking away keys, medicines, or other essentials. Or things like constantly putting you down in public or on social media.
And it can be physical. To make up for differences in strength, abusive partners may try to attack you in your sleep, by surprise, or with weapons and other objects. They may also abuse your children or pets.
What to Do if You’re Being Abused
First, know that you deserve better and that this isn’t your fault. If you’re in an emergency, call 911.
It can be hard to decide whether to stay or leave. That’s why it may help to start with a call to the National Domestic Violence Hotline at 1-800-799-SAFE (1-800-799-7233). Call from a friend’s house or somewhere else where you feel safe.
You can also turn to friends, family, neighbors, your doctor, or your spiritual community.
Also make sure you have an emergency escape plan:
- Hide a set of car keys.
- Pack a bag with keys, extra clothes, important papers, money, and medicines. You might keep it at a friend’s house.
- Have a plan for calling the police in an emergency. You might have a code word, so your kids, family, friends, or co-workers know you’re in danger.
- Know where you’ll go and how you’ll get there.







 By Laura Casey, BSN, RN, Health Partnership Clinic, Infection Control & Occupational Health Coordinator
By Laura Casey, BSN, RN, Health Partnership Clinic, Infection Control & Occupational Health Coordinator


 There are two types of sunscreens available in the United States (US), usually differentiated between mineral (zinc oxide and titanium oxide) and chemical. Zinc and titanium oxide are white metals that reflect the radiation back. However, they are also what we use to make white paint for artists, so they tend to make you look ghostly. If you rub it in well, this can be managed but not eliminated entirely. Chemical (or organic) sunscreens absorb the UVB radiation. Two of them have been implicated in damaging coral reefs, oxybenzone and octinoxate. Anything you wash off your skin will go in the sea eventually, so I prefer to avoid these and especially recommend not taking them for anyone planning a beach vacation.
There are two types of sunscreens available in the United States (US), usually differentiated between mineral (zinc oxide and titanium oxide) and chemical. Zinc and titanium oxide are white metals that reflect the radiation back. However, they are also what we use to make white paint for artists, so they tend to make you look ghostly. If you rub it in well, this can be managed but not eliminated entirely. Chemical (or organic) sunscreens absorb the UVB radiation. Two of them have been implicated in damaging coral reefs, oxybenzone and octinoxate. Anything you wash off your skin will go in the sea eventually, so I prefer to avoid these and especially recommend not taking them for anyone planning a beach vacation.
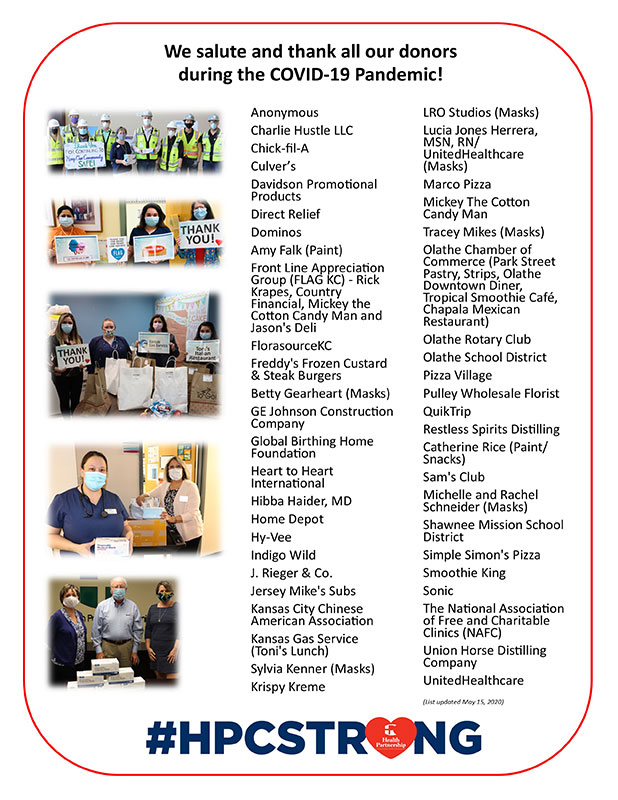
 While times of medical crisis may present themselves as business opportunities for health care organizations, the nature of the pandemic has been the opposite, as patient volumes and health care transactions have been depressed by approximately 50 percent — a seismic shock to statements of operations across the country. In this fashion, the pandemic has demonstrated in a painful way that fee for service still rules the day.
While times of medical crisis may present themselves as business opportunities for health care organizations, the nature of the pandemic has been the opposite, as patient volumes and health care transactions have been depressed by approximately 50 percent — a seismic shock to statements of operations across the country. In this fashion, the pandemic has demonstrated in a painful way that fee for service still rules the day.
 My organization, Health Partnership Clinic, is one of over 1,300 federally qualified health centers in the United States. As such we are a captive audience for the federal government as it communicates its priorities during this pandemic and provides funding. Opportunities exist to continue to improve the alignment of the public health goals of our nation and the population health incentives of health care organizations.
My organization, Health Partnership Clinic, is one of over 1,300 federally qualified health centers in the United States. As such we are a captive audience for the federal government as it communicates its priorities during this pandemic and provides funding. Opportunities exist to continue to improve the alignment of the public health goals of our nation and the population health incentives of health care organizations.




 By
By